Practice Essentials
Ingestion of excessive calcium channel blockers (CCBs) is one of the most potentially lethal prescription drug overdoses. Overdoses of immediate-release CCBs are characterized by rapid progression to hypotension, bradydysrhythmia, and cardiac arrest, while overdoses of extended-release formulations can result in delayed onset of dysrhythmias, shock, sudden cardiac collapse, and bowel ischemia. [1, 2]
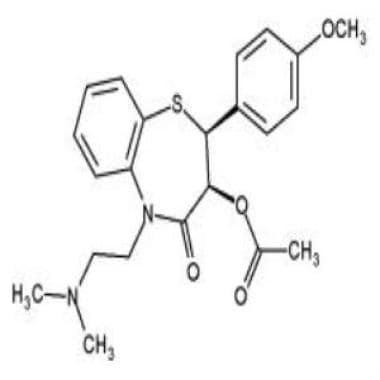
The image below illustrates the chemical structure of the calcium channel blocker diltiazem.
Signs and symptoms
Signs and symptoms of CCB toxicity may include any of the following:
-
Dizziness or lightheadedness
-
Weakness
-
Syncope
-
Chest pain
-
Palpitations
-
Diaphoresis
-
Flushing
-
Peripheral edema
-
Dyspnea
-
Confusion
-
Seizure
-
Headache
-
Nausea and vomiting
Physical examination findings may include the following:
-
Slowed heart rate
-
Hypotension
-
Depressed level of consciousness
See Presentation for more detail.
Diagnosis
Abnormal findings on blood tests in patients with CCB toxicity include the following:
-
Hyperglycemia
-
Hypokalemia
-
Acidosis
On ECG, toxicity from calcium channel blockers may manifest as any of the following:
-
Bradycardia
-
First-, second-, or third-degree atrioventricular (AV) block
-
Any type of bundle-branch block
-
Nonspecific ST-T wave changes
In patients who present after a suicide attempt, and those with a history of co-ingestion, laboratory tests should also include the following:
-
Serum aspirin level
-
Serum acetaminophen level
-
Basic chemistry panel
-
Urine toxicology - Results may suggest significant co-ingestants such as opiates
See Workup for more detail.
Management
Basic supportive care is the first, and possibly most important, mode of management for CCB toxicity: Stabilize airway, breathing, and circulation (ABCs). Correction of acid-base disturbances and electrolyte abnormalities is also important, to optimize cardiac function.
Generally, the recommended duration of clinical observation for asymptomatic patients with significant exposure to CCBs is as follows [3, 4] :
-
Immediate-release products: 6 hours
-
Standard-release products: 6-12 hours
-
Extended-release or once-a-day preparations: 24-36 hours
In cases of intentional overdose, patients who remain asymptomatic after an adequate observation time may be referred for psychiatric evaluation.
Activated charcoal has been demonstrated to significantly absorb immediate-release medications within 1 hour of ingestion and extended-release medications as long as 4 hours after ingestion. [5] Before administration of activated charcoal, protect the patient's airway to prevent vomiting and aspiration.
Consult an American Association of Poison Control Centers–certified regional poison control center in all cases to assist in management, because poisonings can be quite severe and dynamic, and treatment is often complicated and multimodal. For these reasons, when patients are critically ill, besides the initial discussion with the certified specialist in poison information, request to speak with the medical toxicologist on call.
Specific agents used in treatment include the following:
-
IV volume expansion - Normal saline or Ringer lactate
-
Calcium
-
Glucagon
-
Vasopressors (eg, dopamine, epinephrine, norepinephrine)
-
High-dose insulin/euglycemia (HIE) therapy
-
Lipid emulsion therapy
Cardiac pacing may be required.
Calcium
Calcium can be administered IV to patients who present with symptomatic hypotension or heart block, as follows [6, 7, 8] :
-
Calcium gluconate, 30 mL of 10% solution, infused over 10-15 minutes in adults
-
Recommended pediatric dose of calcium gluconate is 60 mg/kg, with a maximum dose of 1 g [9]
-
Calcium chloride (1-4 g) is preferably given via central line, slowly
Glucagon
Reconstitute in D5W, not propylene glycol
Give an initial IV bolus of 5-10 mg; if a positive clinical effect is noted, continue an infusion at 5-10 mg/h
Insulin therapy
High-dose insulin therapy is administered as follows:
-
Infuse one ampule of D50W
-
Give an insulin bolus of 1 U/kg, followed by an infusion of 1-10 U/kg/h
-
Monitor serum potassium and glucose levels every 20-30 minutes
-
D5W infusions usually suffice to maintain glucose levels
See Treatment and Medication for more detail.
Background
Calcium channel blocker (CCB) toxicity is one of the most lethal prescription drug overdoses; therefore, understanding the emergent management of such cases is essential. Overdoses of immediate-release CCBs are characterized by rapid progression to hypotension, bradydysrhythmia, and cardiac arrest. Overdoses of extended-release formulations can result in delayed onset of dysrhythmias, shock, sudden cardiac collapse, and bowel ischemia. [2]
Among the most widely prescribed drugs in the United States, CCBs are used to treat angina, hypertension, and dysrhythmias and to prevent migraines. They are marketed under many brand names, in a range of doses and formulations. Because they are found in many households and children may sometimes mistake them for candy, unintentional ingestion of CCBs is common. In addition, pediatricians have used these agents to treat children (eg, those with congenital heart malformations) for conditions such as dysrhythmias, hypertension, and chronic heart failure. Thus, dosing errors are also a possible source of toxicity in this age group.
These medications have different onsets of action, and many are available in sustained-release forms, all of which complicates the physician's decision regarding the appropriate duration of monitoring for patients with a history of CCB ingestion. (See Presentation and Workup.)
Patients with CCB toxicity should be treated in a well-equipped emergency facility or in an intensive care setting. Numerous strategies for treating patients who have ingested CCBs are available. (See Treatment.)
Pathophysiology
All existing CCBs function by binding to the L-subtype, voltage-sensitive, slow calcium channels in cell membranes. (Mibefradil, the only T-channel calcium blocker, was withdrawn from the market in 1998 because of multiple drug interactions and risk or death.) [10] The L-type calcium channel blockers decrease the flow of calcium into the cells of the cardiac conduction pathway, which leads to an inhibition of phase 0 in cardiac pacemaker cells and slows the phase 2 plateau in Purkinje cells, cardiac myocytes, and vascular smooth muscle cells. In cardiac muscle and vascular smooth, muscle rapid calcium influx causes myosin and actin binding and contraction. The different classes of CCBs, by inhibiting calcium influx, cause decreased myocardial contractility and peripheral arterial vasodilation.
Calcium channel blockers have the following four cardiovascular effects:
-
Peripheral arterial vasodilatation
-
Negative chronotropy (decreased heart rate through sinoatrial node inhibition)
-
Negative dromotropy (decreased cardiac conduction through atrioventricular node inhibition)
-
Negative inotropy (decreased cardiac contractility)
Other physiologic responses to CCB overdose include suppression of insulin release from the pancreas and decreased free fatty acid utilization by the myocardium. These factors produce hyperglycemia, lactic acidosis, and depressed cardiac contractility.
A unique CCB, bepridil, also demonstrates weak cross-reactivity with fast sodium channels and potassium rectifier channels, partially blocking these voltage-gated ion channels, which are responsible for rapid membrane depolarization. There is a propensity towards QTc prolongation and a risk for torsade de pointes.
See the image below.
Etiology
The toxic potential of calcium channel blockers (CCBs) varies with the formulation (eg, immediate-release or sustained-release) and the pharmacologic subclass. The CCBs have a certain degree of tissue specificity, but the drugs do have common properties. CCBs are all well absorbed in the gastrointestinal (GI) system, although diltiazem has extensive first-pass metabolism. The CCBs are substantially bound by plasma proteins and are predominantly metabolized by the liver. Therefore, impaired renal function should not alter CCB metabolism.
CCBs are divided into 3 subclasses. These classes and their effects are as follows [11] :
-
Phenylalkylamines: Affect the atrioventricular (AV) node and peripheral vasculature equally; verapamil is the only available agent in this class
-
Benzothiazines: More negative chronotropic effects than vasoactive; diltiazem is the only available agent in this class
-
Dihydropyridines: Primarily affect the peripheral vasculature, although cardiac toxicity may be observed in overdose; agents in this class are amlodipine, clevidipine, felodipine, isradipine, nicardipine, nifedipine, nimodipine, and nisoldipine
The pharmacokinetics of CCBs are as follows:
-
Amlodipine (Norvasc): Peak plasma level, 6-9 hours; half-life, 30-50 hours
-
Bepridil (Vascor): Peak plasma level, 2-3 hours; half-life, 24 hours
-
Diltiazem immediate release (IR) (Cardizem): Peak plasma level, 2-4 hours; half-life, 3.5-6 hours
-
Diltiazem sustained-release (SR) (Cardizem SR): Peak plasma level, 6-11 hours; half-life, 5-7 hours
-
Diltiazem controlled delivery (Cardizem CD): Peak plasma level, 10-14 hours; half-life, 5-8 hours
-
Diltiazem extended-release (XR or XT) (Dilacor): Peak plasma level, 4-6 hours; half-life, 5-10 hours
-
Felodipine (Plendil): Peak plasma level, 2.5-5 hours; half-life, 11-16 hours
-
Isradipine (DynaCirc): Peak plasma level, 0.5-2 hours; half-life, 8 hours
-
Nicardipine (Cardene): Peak plasma level, 0.5-2 hours; half-life, 2-4 hours
-
Nifedipine immediate release (IR) (Procardia): Peak plasma level, 0.5 hour; half-life, 2-5 hours
-
Nifedipine extended-release (XL) (Procardia XL): Peak plasma level, 7-10 hours; half-life, 7 hours
-
Nimodipine (Nimotop): Peak plasma level, less than 1 hour; half-life, 1-2 hours
-
Nisoldipine (Sular): Peak plasma level, less than 6-12 hours; half-life, 7-12 hours
-
Verapamil immediate release (IR) (Calan Isoptin): Peak plasma level, less than 1-2 hours; half-life, 3-7 hours
-
Verapamil sustained-release (Calan SR, Isoptin SR, Verelan): Peak plasma level, less than 5-11 hours; half-life, 12 hours
Nondihydropyridines
Verapamil
Verapamil (Calan, Isoptin), a phenylalkylamine, has a higher affinity for calcium slow channels in the cardiac conducting system than in peripheral smooth muscle cells; therefore, it causes a greater negative dromotropic and inotropic effect than do other CCBs. Several sustained-release formulations are available (eg, Calan SR, Isoptin SR, Verelan, Covera HS).
Verapamil almost exclusively undergoes hepatic metabolism, yielding a single active metabolite, norverapamil. This compound has 20% of the pharmacologic activity of the parent drug.
Diltiazem
Diltiazem (Cardizem, Cardizem CD, Cardizem SR, Dilacor XR, Teczem, Tiazac) demonstrates an affinity for cardiac conductive tissues and vascular smooth muscle cells, but its clinical response more closely resembles that of verapamil than of nifedipine. Diltiazem mainly undergoes hepatic metabolism, with a large first-pass effect that may differ from patient to patient.
Dihydropyridines
Nifedipine
Nifedipine (Procardia, Procardia XL, Adalat, Adalat CC) is a dihydropyridine. Nifedipine has a relatively high affinity for the calcium channels in the smooth muscle cells of vascular tissue and causes little to no AV nodal interference. At therapeutic doses a slight rebound tachycardia may occur. The primary manifestation of nifedipine-related toxicity is hypotension secondary to loss of systemic vascular resistance. This agent has no active metabolites after hepatic metabolism.
Nicardipine and nimodipine
Nicardipine (Cardene, Cardene SR) and nimodipine (Nimotop) are similar to nifedipine, although they demonstrate greater peripheral vascular smooth muscle effects. They may have small, negative inotropic effects. Nicardipine and nimodipine are predominantly metabolized by the liver. They do not exhibit a large first-pass effect, as is observed with other CCBs. Nimodipine has selectivity for the cerebral vasculature because of its high lipid solubility and ability to cross the blood-brain barrier; it has been approved for use in the treatment of cerebral ischemia after subarachnoid hemorrhage. Nicardipine is also available as an IV formulation for the control of hypertension.
Amlodipine
Amlodipine (Norvasc) has a long half-life of 30-50 hours. [12] The clinical effects of amlodipine are similar to those of nicardipine. Amlodipine’s long duration of action increases the risk of morbidity and mortality from an overdose.
Felodipine
Felodipine is highly protein-bound and exhibits a half-life of 11-16 hours. Because of protein binding, the drug’s elimination is prolonged. Due to its hypotensive effect, felodipine may cause a reflex tachycardia.
Isradipine
Isradipine (DynaCirc) is similar to felodipine. However, it has a smaller volume of distribution and a half-life of 8 hours. It has some inhibition at the sinoatrial node and therefore has less reflex tachycardia than other dihydropyridines.
Nisoldipine
Nisoldipine (Sular), a dihydropyridine, is highly metabolized, which results in only 1 active metabolite that has about 10% the activity of the parent compound. Nisoldipine elicits predominantly peripheral hemodynamic effects. It decreases systemic vascular resistance and blood pressure. It has a relatively high affinity for the calcium channels in the smooth muscle cells of vascular tissue and causes little to no AV nodal interference.
Clevidipine
Clevidipine (Cleviprex) is a dihydropyridine L-type CCB administered intravenously. It is rapidly distributed and metabolized and therefore has a very short half-life (terminal half-life of approximately 15 min). L-type calcium channels mediate the influx of calcium during depolarization in arterial smooth muscle. Clevidipine reduces mean arterial blood pressure by decreasing systemic vascular resistance. It does not reduce cardiac filling pressure (preload), confirming a lack of effects on the venous capacitance vessels.
Epidemiology
United States statistics
In 2021, the American Association of Poison Control Centers (AAPCC) reported 6162 single exposures to calcium antagonists, resulting in 37 deaths and 119 major outcomes; 1228 exposures occurred in children younger than 6 years. [13] The past decade has seen only a minimal decline in the percentage of pediatric exposures to CCBs of all cases called to poison control centers nationally. [14, 15, 16, 17, 18, 19]
Race-, sex-, and age-related differences in incidence
Although CCB ingestion has no race predilection among young children, racial trends mirror suicide attempt statistics among adolescents. In young children, a male predilection for CCB toxicity is observed. In adolescents, the sex predilection again mirrors suicide attempt statistics, with more females than males ingesting calcium channel blocker agents.
CCB ingestions show a bimodal distribution in the pediatric age range. Infants and toddlers often unintentionally ingest tablets that they mistake for food or candy. Teenagers ingest CCBs as a suicide gesture.
Prognosis
Prognosis in calcium channel blocker (CCB) toxicity depends on the following:
-
Amount and formulation of drug ingested
-
Co-ingestions
-
Patient's age
-
Underlying disease states
-
Specific treatments
-
Initial cardiac rhythm
-
Time elapsed before treatment begins
-
Specific treatments
-
Use of a pacemaker and time before it is placed
In 2021, the American Association of Poison Control Centers (AAPCC) reported that calcium channel blockers (CCBs) were the sixth leading cause of fatality. [19]
Complications
Complications relating to CCB toxicity include the following:
-
Dysrhythmias
-
Seizure
-
Coma
-
Anoxic encephalopathy from prolonged central nervous system (CNS) hypoxia
-
Ileus
-
Bowel infarction or perforation from mesenteric hypotension
-
Noncardiogenic pulmonary edema
-
Aspiration pneumonia
-
Death
CCBs, especially sustained-release formulations, can be lethal in toddlers; a few rare ingestions of a single pill have been documented to cause death. [17, 20, 21] Therefore, whenever a physician or parent suspects that a child has taken a CCB, aggressive treatment in a well-equipped hospital setting should be rapidly initiated.
Patient Education
Educate parents and grandparents who take calcium channel blocker (CCB) medications about the importance of keeping these drugs out of the reach of children. CCBs should be kept in childproof bottles. In addition, all homes should have the number of the poison control center (800-222-1222) posted on or near their telephones for use in an emergency. Calling this number connects the caller to his or her regional poison control center.
For patient education information, see First Aid for Poisoning in Children and Child Safety Proofing.
-
Calcium channel blocker; diltiazem.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Prehospital Management
- Emergency Department Management
- Indications for Inpatient Evaluation
- Gastrointestinal Decontamination
- Treatment of Hypotension
- Calcium Therapy
- Glucagon Therapy
- Vasopressor Therapy
- Insulin Therapy
- Investigational Therapies
- Procedures
- Diet and Activity
- Consultations
- Transfer
- Show All
- Medication
- Questions & Answers
- Tables
- References